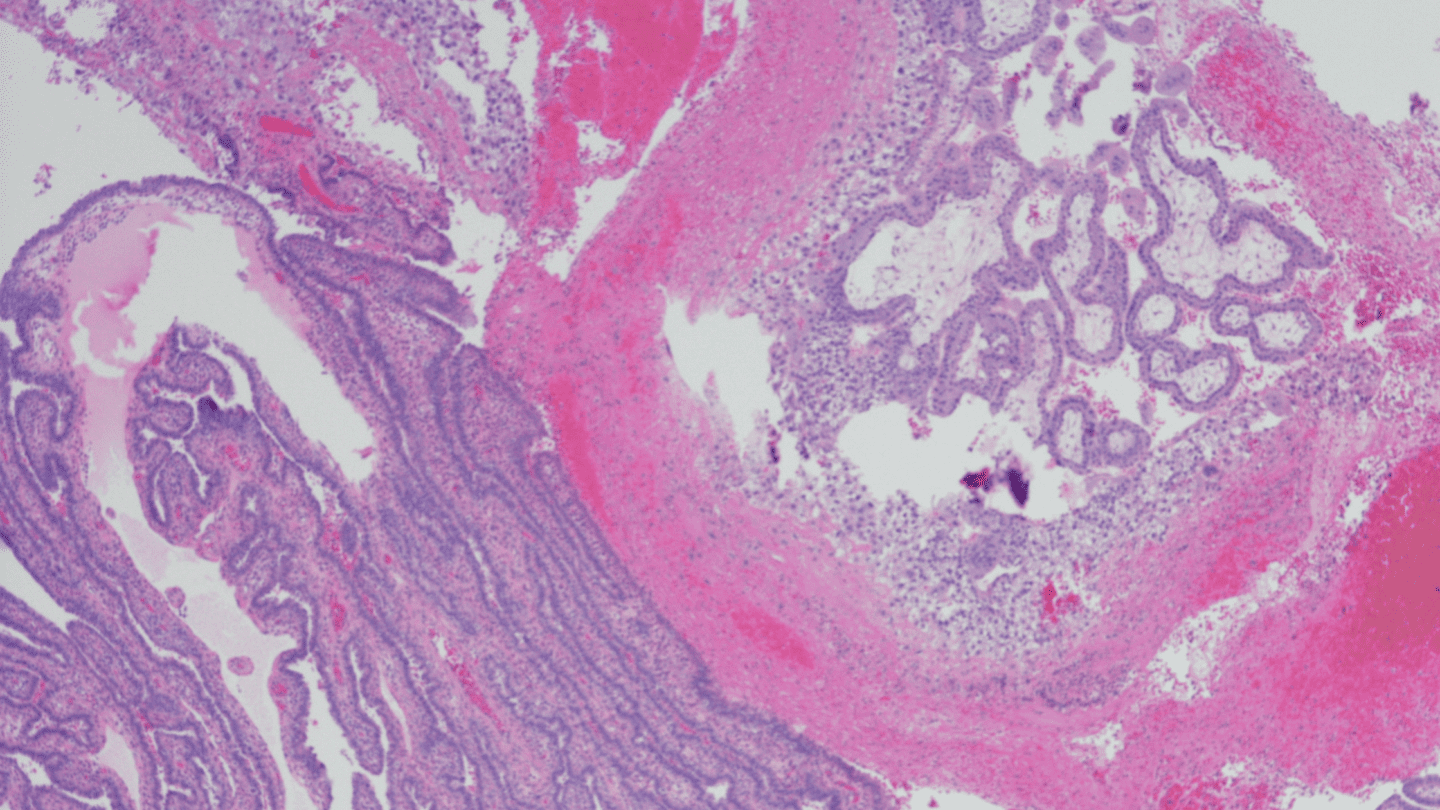
A fibroid diagnosis can be scary. The uterine tumors can be painful, and not much is known about where they come from and what causes to grow. Up to 80% of women and people with a will get at some point in their life1, yet a surprising number of people haven’t heard of them. In some cases, doctors may opt to remove the entirely to treat . But today, a growing number of treatment options mean there are many less-invasive options for treatment.
What are ?
Fibroids are benign tumors that grow on the walls of your . Medical professionals sometimes refer to them as or myomas. A lot of people that have don’t even know they have them, and that’s fine — it’s the symptoms they cause that can become problematic.
Fibroids are frustratingly understudied, as are so many reproductive health issues. Even today, the most common fibroid treatment offered to patients is simply cutting out the entirely, despite the availability of other options.2 Another prime example: The system for classifying was developed in 1918, and hasn’t been updated since.3
What causes ?
Researchers know surprisingly little about what causes to grow. So far, it seems like a complex combination of factors are at play. Research has found links between and:
- Hormones. Studies have found that people who use that includes and , like The Pill and hormonal IUDs, are 20% less likely to have .4 Other researchers have proposed that exposure to endocrine-disrupting chemicals — pollutants that mess with your hormones — increase risk.5
- Genes. If you have a close relative with , your risk is much higher. Researchers have identified a myriad of s that can increase your likelihood for . Factors that can mess with your , called epigenetics, also can make them more likely.6
- Age. The odds of developing rise as you approach . Most people with are first diagnosed in their 30s or 40s, and the risk of is highest when you’re in your 50s.7 After , the risk drops off and may even shrink and disappear, thanks to the hormonal changes happening in your body.
A number of studies have linked to other factors, such as:
- Exposure to plastics and chemicals8
- Consumption of soy milk, food additives, sweeteners, and preserved foods8
- Obesity
- Vitamin D9
- Hypertension10
The majority of these studies are small, and still need to be repeated in larger, more controlled settings before we can understand how important they really are.
Researchers have found that Black women get three times more often than white women, and that when they do, they get them at a younger age, they’re larger, their symptoms are more severe, and their risk of complications is higher.11 The reason why Black women get more often is still a medical mystery, but some researchers suspect it relates to genetics and underlying health conditions. The lack of attention on the issue is just one of many examples of long-running racial disparities in the healthcare system and beyond.
Like what you’re reading? Get the latest straight to your inbox 💌
What are the symptoms?
Fibroids don’t always cause symptoms, and a lot of people who have them don’t even know they’re there. But for some, they can cause a wide range of troubles, including:
- pelvic or lower back pain
- heavy periods characterized by more bleeding than is normal for you
- increased urination or incontinence
- a feeling of fullness in the abdomen
- pain during intercourse
- pregnancy complications or
It’s important to see your ob-gyn if you think you might have . Some fibroid symptoms can feel similar to those caused by ovarian cysts and . These other conditions need different treatments, so it’s important to get an accurate diagnosis to alleviate your symptoms.
Doctors can check for during your routine pelvic exam. If they need to take a closer look, they might bring in heavy machinery, like ultrasound machines or MRIs.
What’s the best treatment for ?
Luckily, don’t typically pose a big danger if they’re dealt with properly, and there are a wide range of treatment options available. If your symptoms are minimal, your doctor might even recommend leaving them alone. They call this “watchful waiting.” This fibroid treatment, or non-treatment, is an especially common practice for older people, since often shrink and disappear after .
If are causing you pain or other symptoms, your doctor will likely recommend treatment, which ranges from non-invasive medication to surgical removal. Here are some of the most common fibroid treatment options.
Hormonal treatments for
There’s some evidence that hormonal contraceptives, like the pill and certain s (IUDs) can help manage some fibroid symptoms like heavy bleeding.12 Some studies have also shown that the hormones progesterone and affect fibroid growth.13 Doctors may prescribe drugs that change how these hormones are produced or transmitted in the body to alleviate symptoms and shrink .
Gonadotropin-releasing (GnRH) analogs
A class of drug called gonadotropin-releasing hormone (GnRH) analogs mimic hormones in the body to simulate the onset of .14 Research shows it’s a reliable way to shrink , but side effects of the drug, like bone loss, makes it a bad option for long-term use. Doctors most often prescribe GnRH drugs temporarily, for instance to shrink before a surgery to remove them completely.
Removing
When are causing problems, like interfering with your ability to have children, your doctor may recommend procedures to remove or destroy the growths. One option is to use focused ultrasound to heat and destroy fibroid cells, often guided by an MRI. Doctors may also recommend uterine artery embolization, in which they inject tiny particles into the arteries that supply blood to the .15 Slowing the blood flow kills the while leaving the other tissues in the intact.
Surgeons can directly cut out , too, which is called a myomectomy. To do this surgery, doctors create a small incision and use small, flexible tools to cut out the growths. This procedure comes with minimal risks, but it’s not a permanent solution — can grow back over time.
For years, doctors have most commonly recommended hysterectomies as treatment for symptomatic — removing the entirely.2 It’s effective, but it’s the most extreme option. Removing a is a major surgery that comes with long recovery times, can come with complications, and eliminates a person’s ability to have children.
Some people feel emotionally connected to their , even without a desire to have children, and prefer not to part with it. So although a may be the right choice for some people, it’s not something you should feel pressured into. It’s typically best to have an open conversation with your doctor about the alternatives.
Closing the research gap
Scientists agree that fibroids need more study.16 As with other aspects of reproductive health, we’re still waiting on good, solid science to show us what causes and how we can best treat and prevent them. Some of that work is underway now, but we have a long way to go before we close this portion of the medical research gap.
Help us spread the word about ! Share this post with your family and friends.
-
- New York Department of Health (May 2013) Uterine Fibroids. Accessed Aug 3, 2021.
- Giuliani E, As‐Sanie S, Marsh EE. (2020) Epidemiology and management of uterine fibroids. International Journal of Gynecology & Obstetrics. doi: 10.1002/ijgo.13102
- Gliklich RE, Leavy MB, Velentgas P, et al. (Mar 2011) Identification of Future Research Needs in the Comparative Management of Uterine Fibroid Disease. Effective Healthcare Research Report. 31.
- Kwas K, Nowakowska A, Fornalczyk A, et al. (2021) Impact of Contraception on Uterine Fibroids. Medicina. 57(7):717. doi: 10.3390/medicina57070717
- Bariani MV; Rangaswamy R, Siblini H, et al. (Dec 2020) The role of endocrine-disrupting chemicals in uterine fibroid pathogenesis. Current Opinion in Endocrinology, Diabetes and Obesity. 27(6):380-387.doi: 10.1097/MED.0000000000000578
- Toprani S & Mane V. (Jan 2021) Role of DNA damage and repair mechanisms in uterine fibroid/leiomyomas: A review. Biology of Reproduction. 104(1):58-70. doi: 10.1093/biolre/ioaa157
- Office on Women’s Health. (Apr 2019) Uterine Fibroids. U.S. Department of Health and Human Services. Accessed Aug 3, 2021.
- Shen Y, Xu Q, Xu J, Ren ML, Cai YL. (2013) Environmental exposure and risk of uterine leiomyoma: an epidemiologic survey. European Review for Medical and Pharmacological Sciences. 17(23):3249-56.
- Al-Hendy A, Badr M. (Jul 2014) Can vitamin D reduce the risk of uterine fibroids? Women’s Health. 10(4):353-8. doi: 10.2217/whe.14.24.
- Luoto R, Rutanen EM, Auvinen A. (Apr 2001) Fibroids and hypertension. A cross-sectional study of women undergoing hysterectomy. Journal of Reproductive Medicine. 46(4):359-64.
- Stewart EA, Nicholson WK, Bradley L, Borah BJ. (Oct 2013) The burden of uterine fibroids for African-American women: results of a national survey. Journal of Women’s Health. 22(10):807-16. doi: 10.1089/jwh.2013.4334
- Moroni RM, Martins WP, Dias SV, et al. (Feb 2015) Combined oral contraceptive for treatment of women with uterine fibroids and abnormal uterine bleeding: a systematic review. Gynecologic and Obstetric Investigation. 79(3):145-52. doi: 10.1159/000369390.
- Moravek MB, Bulun SE. (Aug 2015) Endocrinology of uterine fibroids: steroid hormones, stem cells, and genetic contribution. Current Opinion in Obstetrics & Gynecology. 27(4):276-83. doi: 10.1097/GCO.0000000000000185.
- Hodgson R, Bhave Chittawar P, Farquhar C. (Oct 2017) GnRH agonists for uterine fibroids. Cochrane Database of Systematic Reviews. 10:CD012846. doi: 10.1002/14651858.CD012846
- Mayo Clinic Staff. (Jul 2021) Uterine artery embolization. Accessed August 3, 2021.
- Al-Hendy A, Myers ER, Stewart E. (Nov 2016) Uterine Fibroids: Burden and Unmet Medical Need. Seminars in Reproductive Medicine. 35(6):473-480. doi: 10.1055/s-0037-1607264.