If you’re wondering whether you have , you’re not alone.
Endometriosis is a common gynecological condition that affects about 11% of American women1 between ages 15 and 44.
Any woman can develop , but people may have a higher risk if they2:
- Have a close biological relative who shares the condition
- Started their period before age 11
- Have monthly cycles of less than 27 days
- Have heavy periods that last longer than 7 days
What is ?
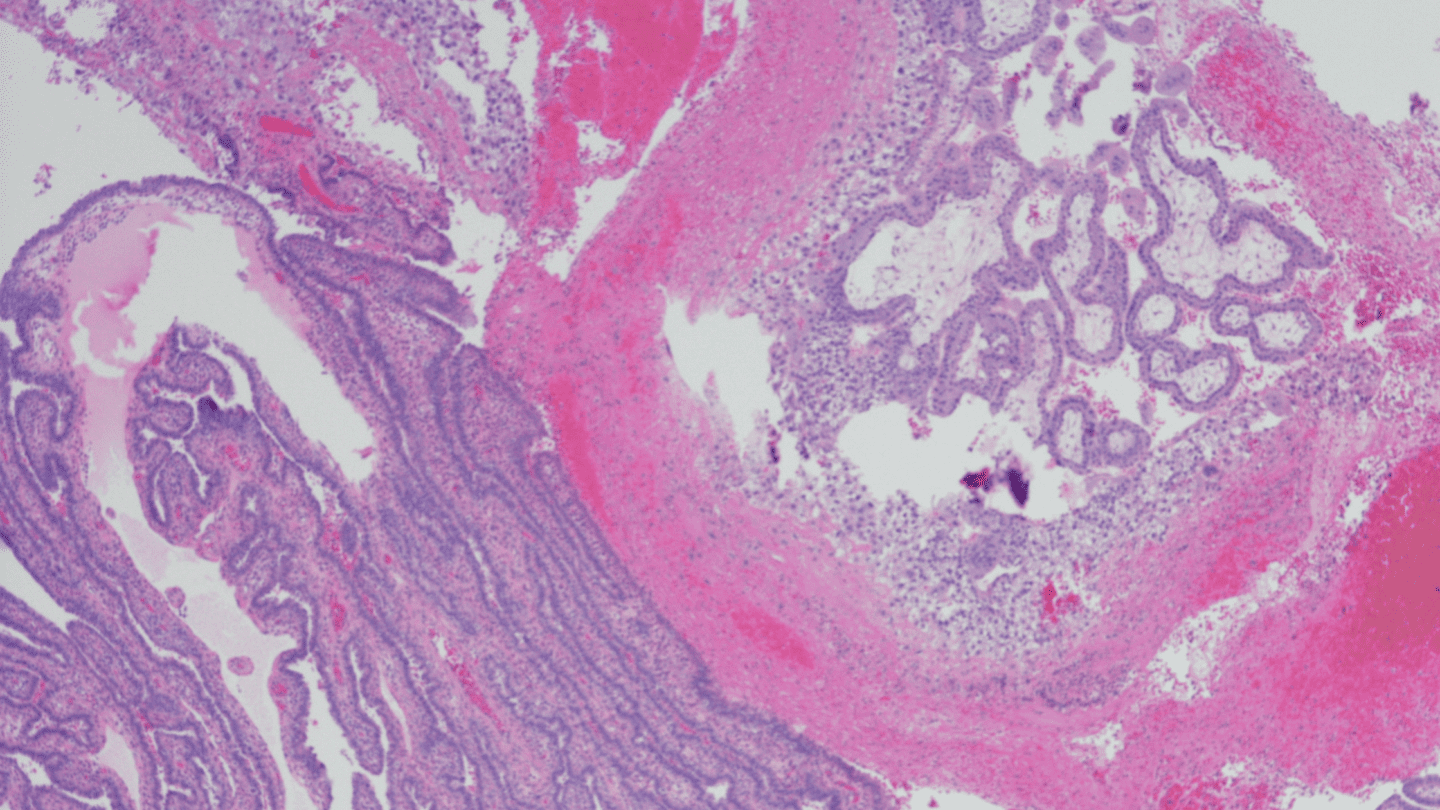
When a person has , an endometrium-like tissue (often referred to as implant, nodule, or lesion) is found on reproductive organs such as3-4:
- Ovaries
- Fallopian tubes
- Tissues that hold the in place
- Outer surface of the
- Vagina, cervix, , bowel, bladder, or rectum
- Abdominal cavity
In addition to causing pain, sometimes makes it harder for people to get pregnant.
Signs and symptoms of
Not everyone presents all symptoms or the exact same symptoms, but some of the common signs may include1,4:
- Pain (like excessive menstrual cramps in your abdomen or lower back)
- Bleeding or between periods
- Abnormal or heavy menstrual flow
- Infertility (detailed more in the next section)
- Gastrointestinal problems
If you are experiencing any of these symptoms, keep a journal of what pain occurs and when before seeing your doctor. This may help clarify whether or not you have , and help you come with more evidence than just generic pain.
Like what you’re reading? Get the latest straight to your inbox 💌
How is diagnosed?
In order to receive a diagnosis for 5, your healthcare provider or gynecologist will:
- Ask questions about your medical history (including family medical history)
- Conduct a physical examination and pelvic exam
- Perform an ultrasound, or MRI scan to view internal organs
However, the only way to get a completely certain diagnosis of is for a doctor to use laparoscopy and perform a biopsy on unusual tissue.
Laparoscopy uses a laparoscope, which is a thin tube with a camera at the end. In this minor medical procedure, your healthcare provider would create a small incision and insert the laparoscope6 in order to understand the size, location, and extent of endometrial growths.
What causes ?
Long story short, the causes of are not definitively clear. However, there are a few different theories4:
- While you’re on your period, some of the tissue may back up through your fallopian tubes into the abdomen, where it attaches and then grows, sort of like a reverse period.
- Endometrial tissue may travel and implant itself through lymphatic channels or blood
- Cells in any location may transform into endometrial cells.
Other potential causes may include1:
- Immune system problems
- Genetic factors
- Hormones
- Certain surgeries
How is treated?
Most healthcare providers use “watchful waiting”4 to see how the health condition progresses. That means repeating tests or allowing some time to pass before making major health interventions.
There are also several types of medicine you can take to address symptoms of , such as:
Pain medication
Nonsteroidal anti-inflammatory drugs7 like ibuprofen can help you manage pain from . Other over-the-counter analgesics like acetaminophen, aspirin, and naproxen may help with the pain as well.
Extended cycle or continuous cycle
Extended cycle 8 is a daily combination pill of and that allows you to have your period only once every three to four months. Continuous cycle , such as the combination pill or mini pill9, may also be used to treat the symptoms of .1 Some recent studies have come out that suggest progestin-only (mini) pills might be better10 than combination pills in treating .
Hormonal IUD
A hormonal IUD such as Mirena can be used to treat by suppressing tissue growth, reducing bleeding, and easing pelvic inflammation. However, this is a more recently employed, off-label use that requires additional research and clinical trials to fully validate.11
GnRH agonist
Also known as gonadotropin releasing , GnRH agonists are modified versions of a naturally occurring . By reducing the level of made by the , this can shrink the .12
However, GnRH should not be taken for longer than six months because it can cause other severe side effects13 such as bone loss. It can also cause temporary , so it would not be a good choice for those who are seeking to get pregnant.
Danazol
Danazol is a synthetic derivative of .14 Treatments of danazol15 usually last between three to six months, but may have side effects such as increased body hair and acne.
Surgery
Surgery is only used for severe symptoms of .1 A surgeon can locate where the is and remove it. Some patients resume taking hormonal treatments, such as oral contraceptives, after surgery to prevent the from recurring.16 However, as of 2016, there is limited clinical evidence to suggest this works.17
Identifying and managing might feel like an overwhelming task. But if you do receive a diagnosis, there are many different treatments available that can help ease your symptoms.
adyn specializes in helping people find the right for their bodies.
If you have been diagnosed with and want to learn about your options, adyn can help.
-
- Office on Women’s Health. (2019b, April 1). Endometriosis. https://www.womenshealth.gov/a-z-topics/endometriosis
- National Institutes of Health. (2021). What are the risk factors for endometriosis? https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/at-risk
- National Institutes of Health. (2020, February 21). About Endometriosis. https://www.nichd.nih.gov/health/topics/endometri/conditioninfo
- Johns Hopkins Medicine. (2021). Endometriosis. https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- A, H. (2011, June 1). Invasive and non-invasive methods for the diagnosis of endometriosis. NCBI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880548/
- Office of Communications. (2020, February 2). How do healthcare providers diagnose endometriosis? National Institutes of Health. https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/diagnose
- Endometriosis UK. (2021). Pain relief for endometriosis. https://www.endometriosis-uk.org/pain-relief-endometriosis
- University of Michigan Health. (2019, July 18). ethinyl estradiol and levonorgestrel (extended-cycle). https://www.uofmhealth.org/health-library/d03242t1
- Centers for Disease Control and Prevention. (2017, February 1). Combined Hormonal Contraceptives. https://www.cdc.gov/reproductivehealth/contraception/mmwr/spr/combined.html
- Casper, R. F. (2017). Progestin-only pills may be a better first-line treatment for endometriosis than combined estrogen-progestin contraceptive pills. American Society for Reproductive Medicine. Published. https://pubmed.ncbi.nlm.nih.gov/28162779/
- Wood, R. (2021). Mirena. Https://Endometriosis.Org/Treatments/Mirena/. https://endometriosis.org/treatments/mirena/
- Rafique, S. (2018). Medical management of endometriosis. National Library of Medicine. Published. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5794019/
- LiverTox. (2018). Gonadotropin Releasing Hormone (GnRH) Analogues. LiverTox. Published. https://www.ncbi.nlm.nih.gov/books/NBK547863/
- National Cancer Institute, Drug Dictionary. danazol. https://www.cancer.gov/publications/dictionaries/cancer-drug/def/danazol?redirect=true
- MedlinePlus. (2017, May 24). Danazol. https://medlineplus.gov/druginfo/meds/a682599.html
- National Institutes of Health. (2020, February 21). What are the treatments for endometriosis? https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/treatment
- Somigliana, E. (2017). Postoperative hormonal therapy after surgical excision of deep endometriosis. National Library of Medicine. Published. https://pubmed.ncbi.nlm.nih.gov/27067871/